Polycythemia and Testosterone Replacement Therapy: Understanding the Link
Testosterone Replacement Therapy (TRT) has become an increasingly common treatment for men experiencing low testosterone levels due to aging or hypogonadism. While TRT can significantly improve quality of life by alleviating symptoms such as fatigue, depression, and decreased libido, it is not without potential side effects. One such side effect is polycythemia, a condition characterized by an increased number of red blood cells. This article explores the relationship between TRT and polycythemia, including the mechanisms, risks, and management strategies.
What is Polycythemia?
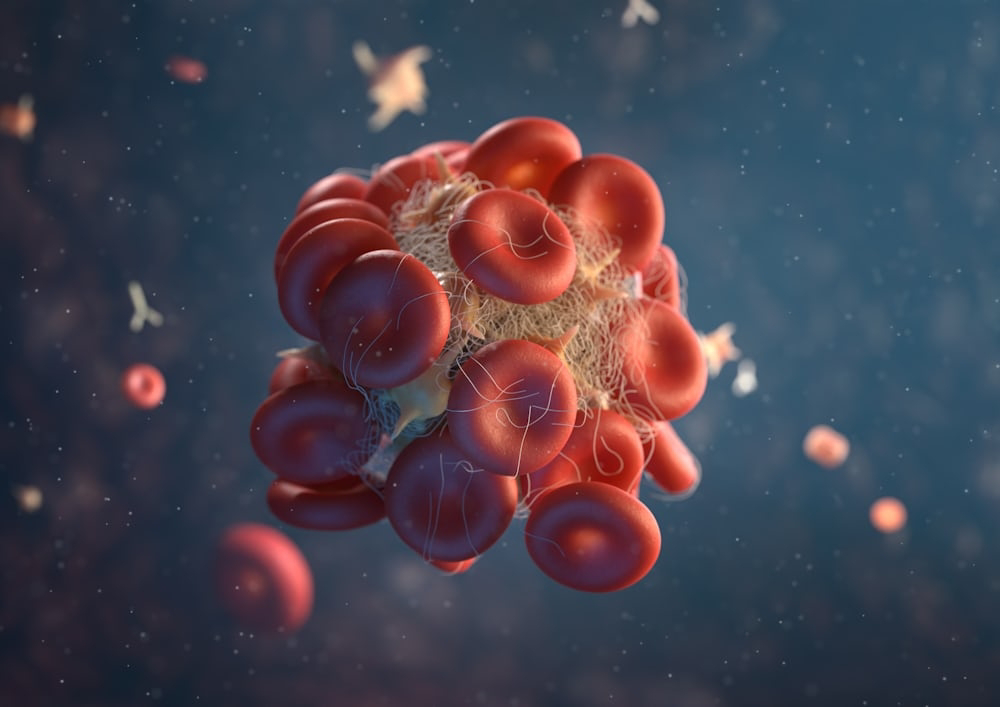
Polycythemia is defined by an elevated hematocrit (Hct), hemoglobin (Hb), and red blood cell (RBC) count. Hematocrit refers to the proportion of blood volume occupied by red blood cells. There are two main types of polycythemia:
- Primary Polycythemia (Polycythemia Vera): A rare blood disorder where the bone marrow produces too many red blood cells due to a genetic mutation.
- Secondary Polycythemia: Caused by factors outside the bone marrow that lead to increased red blood cell production. Common causes include chronic hypoxia (e.g., from smoking or high altitudes) and certain tumors. TRT-related polycythemia falls into this category.
Testosterone Replacement Therapy and Polycythemia
Mechanisms
Testosterone stimulates erythropoiesis, the process of red blood cell production, primarily through its effects on erythropoietin (EPO). EPO is a hormone produced by the kidneys that promotes the formation of red blood cells in the bone marrow. TRT increases testosterone levels, which in turn boosts EPO production, leading to elevated red blood cell counts.
Several studies have shown that TRT can increase hematocrit levels, sometimes pushing them beyond the normal range. This effect can occur regardless of the method of testosterone administration, including injections, gels, and patches.
Risk Factors
Not all men on TRT develop polycythemia. Several factors can influence the risk:
- Dosage and Duration: Higher doses and longer duration of TRT are associated with a greater risk of developing polycythemia.
- Route of Administration: Injectable forms of testosterone are more likely to cause polycythemia compared to transdermal methods, due to the peaks and troughs in testosterone levels that injections produce.
- Baseline Hematocrit: Men with higher baseline hematocrit levels are at a greater risk of developing polycythemia during TRT.
- Age: Older men are more susceptible to the hematopoietic effects of testosterone.
Clinical Implications
Polycythemia can lead to increased blood viscosity, which raises the risk of thromboembolic events such as deep vein thrombosis (DVT), pulmonary embolism, and stroke. These complications are serious and potentially life-threatening, making it crucial to monitor hematocrit levels in men undergoing TRT.
Monitoring and Management
Monitoring
Regular monitoring of hematocrit levels is essential for men on TRT. The Endocrine Society recommends checking hematocrit before initiating therapy, at 3-6 months after starting TRT, and then annually. More frequent monitoring may be necessary for men with elevated baseline hematocrit levels or those who develop polycythemia.
Management Strategies
- Dose Adjustment: Reducing the dose of testosterone can help lower hematocrit levels.
- Switching Administration Routes: Transitioning from injectable to transdermal testosterone can mitigate peaks in testosterone levels and reduce the risk of polycythemia.
- Therapeutic Phlebotomy: This procedure involves removing blood to decrease hematocrit levels. It is similar to donating blood and can be an effective way to manage TRT-induced polycythemia.
- Discontinuation of TRT: In severe cases, stopping testosterone therapy may be necessary.
While TRT offers significant benefits for men with low testosterone, it is important to be aware of potential side effects such as polycythemia. Understanding the mechanisms, risk factors, and management strategies can help healthcare providers and patients navigate this complication. Regular monitoring and proactive management are key to ensuring the safe and effective use of TRT.
References
- Bachman, E., Travison, T. G., Basaria, S., Davda, M. N., Guo, W., Li, M., ... & Bhasin, S. (2010). Testosterone induces erythrocytosis via increased erythropoietin and suppressed hepcidin: evidence for a new erythropoietin/hemoglobin set point. J Gerontol A Biol Sci Med Sci, 65(10), 1181-1189.
- Rhoden, E. L., & Morgentaler, A. (2004). Risks of testosterone-replacement therapy and recommendations for monitoring. New England Journal of Medicine, 350(5), 482-492.
- Basaria, S., Coviello, A. D., Travison, T. G., Storer, T. W., Farwell, W. R., Jette, A. M., ... & Bhasin, S. (2010). Adverse events associated with testosterone administration. New England Journal of Medicine, 363(2), 109-122.
- Morales, A., Bebb, R. A., Manjoo, P., Wassersug, R. J., & Hamilton, L. D. (2015). Diagnosis and management of testosterone deficiency syndrome in men: clinical practice guideline. Canadian Medical Association Journal, 187(18), 1369-1377.




Comments
Post a Comment